Post-Traumatic Stress Disorder (PTSD) is a serious mental health condition that can occur after someone experiences a traumatic event, such as an accident, assault, natural disaster, or combat exposure. The psychological toll of trauma can leave lasting impressions on the mind, influencing thoughts, emotions, and behavior in ways that interfere with everyday life. Understanding what is PTSD is crucial for anyone who may be experiencing symptoms or knows someone who is.
In this article, we’ll explore PTSD meaning, its symptoms, causes, and treatment options, addressing questions like “is PTSD treatable” and “what is PTSD like” for those affected. We’ll also discuss PTSD prevalence and touch on recent Ohio mental health statistics to highlight the growing importance of PTSD awareness.
What is PTSD?
Post-Traumatic Stress Disorder (PTSD) is a mental health condition that develops in response to witnessing or experiencing a traumatic event. Trauma affects the mind and body, leaving many struggling to recover even long after the event has ended. According to the Ohio Health Policy Institute’s Data Snapshot, PTSD is one of the many mental health issues that have been increasingly prevalent, particularly after the onset of the COVID-19 pandemic. The statistics show a marked rise in cases of anxiety, depression, and trauma-related disorders across Ohio and the United States.
The definition of PTSD according to the Diagnostic and Statistical Manual of Mental Disorders, 5th edition (DSM-5; American Psychiatric Association, 2013) is that it is a mental health condition that can occur after a life-threatening event(s): death or threatened death, serious injury, or sexual violence via: 1) directly experiencing it, 2) witnessing the event in person as it occurred to others, 3) learning it happened to someone you were close to, 4) repeated or extreme exposure to aversive details of the events, often through one’s job (e.g., first responders). Symptoms may include recurring flashbacks, hypervigilance, avoidance of reminders of the trauma, and difficulty sleeping or concentrating. Psychology Today explains that PTSD symptoms can range from subtle emotional triggers to more overt behavioral changes, including irritability, aggression, or social withdrawal (Psychology Today).
PTSD Prevalence
PTSD affects individuals across all demographics, though certain populations, like veterans and survivors of assault, may experience it more frequently. PTSD prevalence in Ohio and nationally reflects a significant portion of the population. Studies estimate that around 6-7% of the U.S. population will experience PTSD in their lifetime, though prevalence rates may vary depending on factors like gender, occupation, and trauma exposure. The Ohio Health Policy Institute found that Ohioans, especially healthcare workers and first responders, saw an increase in mental health issues related to stress and trauma, with PTSD being a key concern.
Symptoms of PTSD: How to Know if You Have PTSD
Recognizing signs of PTSD is a vital step toward seeking help. While everyone’s reaction to trauma is unique, there are common indicators that suggest someone may be struggling with post-traumatic stress disorder:
- Re-experiencing Symptoms: Flashbacks, intrusive memories, nightmares, and severe emotional distress and/or physiological reactions (like heart racing or sweating or a panic attack) when reminded of the traumatic event.
- Avoidance: Steering clear of places, people, or activities that remind you of the trauma. Also avoiding memories, thoughts, or emotions related to the trauma.
- Negative Changes in Thinking and Mood: Persistent feelings of fear, horror, anger, guilt, or shame; difficulty experiencing positive emotions; trouble remembering important parts of the event, negative views about self, others, or the world, and blaming self or others.
- Hyperarousal: Increased irritability, difficulty sleeping, being easily startled, feeling constantly “on guard,” and difficulty concentrating.
If you’ve noticed these symptoms in yourself or someone you know, it’s essential to understand what PTSD is like and to recognize that these symptoms are not simply “bad days” but rather signs of a condition that may benefit from treatment.
What Causes PTSD?
PTSD stems from exposure to a traumatic event, but what causes PTSD is a complex interaction among an individual’s biological, psychological, and sociocultural factors. Most people exposed to a traumatic event will experience some of the above symptoms. The symptoms are normal reactions to life-threatening situations. For many people, the symptoms reduce over time without treatment. A strong social support network can reduce the likelihood of PTSD occurring. However, for some individuals, they experience many of the above symptoms for at least a month and the symptoms interfere with their daily functioning. These symptoms can also be worsened by stress with work, family, finances, health, etc. Taken together, only some individuals exposed to trauma develop PTSD. Risk factors for PTSD include the intensity of the trauma, previous mental health history, a lack of social support, and even biological factors that affect how the brain processes stress.
Acute Stress Disorder vs PTSD: After experiencing trauma, some people may develop acute stress disorder (ASD), which shares many symptoms with PTSD. However, ASD is typically a short-term reaction that lasts for less than a month, whereas PTSD is diagnosed when symptoms persist for more than a month. Early intervention for ASD may help prevent it from evolving into PTSD.

Is PTSD a Mental Illness?
Yes, PTSD is a mental illness, recognized by mental health professionals and classified in the Diagnostic and Statistical Manual of Mental Disorders, now in its 5th edition (DSM-5). It’s also categorized as a trauma- and stressor-related disorder rather than an anxiety disorder, though it shares some similarities with anxiety disorders and depression.
Many people wonder, is PTSD an anxiety disorder? While PTSD does involve heightened stress responses and hypervigilance, it is not classified as a traditional anxiety disorder. Instead, it exists in its own category, emphasizing the unique effects trauma has on mental health.
How is PTSD Diagnosed?
Diagnosis of PTSD typically involves a comprehensive assessment by a qualified mental health professional, who may use a combination of clinical interviews, such as the Clinician Administered PTSD Scale (CAPS-5; Weathers, Blake, et al., 2013) or Structured Clinical Interview for DSM (SCID) and self-report questionnaires, such as the PTSD Checklist for DSM-5 (PCL-5; Weathers, Litz, et al., 2013). The process often involves being asked questions about traumatic event(s), the symptoms experienced since the traumatic event(s), and how these symptoms affect daily life. Reliable diagnosis is key to receiving effective psychological treatment for post-traumatic stress.
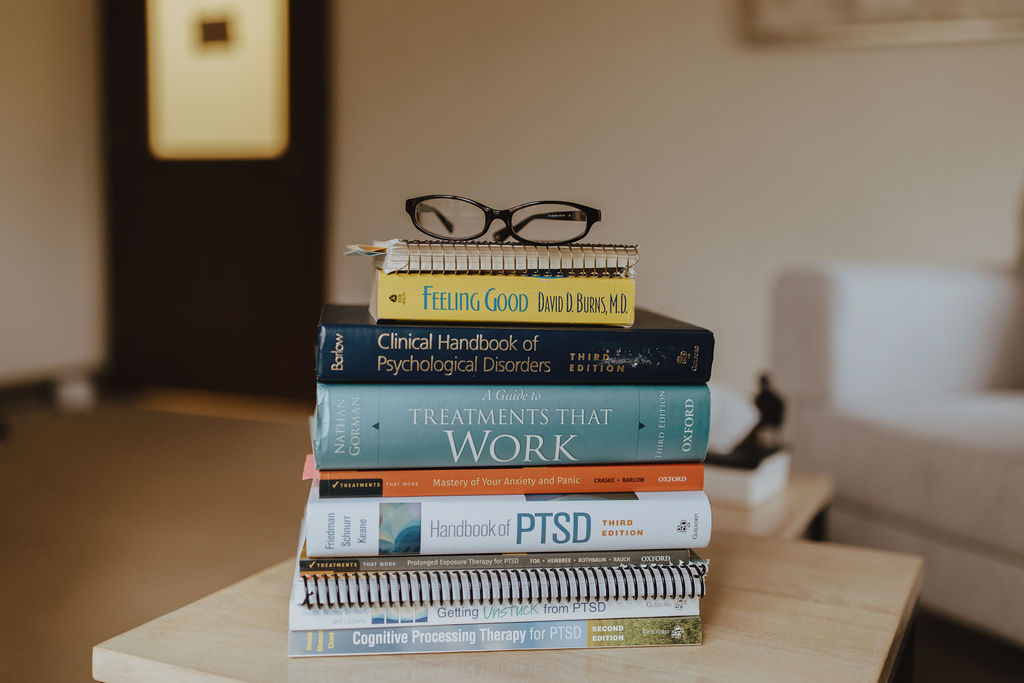
PTSD Therapies and Treatment Options
Is PTSD treatable? Absolutely. While PTSD can be challenging to live with, many effective treatment options are available. PTSD therapies vary in approach, and a qualified mental health provider can recommend the best course of action based on an individual’s symptoms and needs. Common treatments include:
- Cognitive Processing Therapy (CPT): Focuses on changing trauma-related thoughts that are getting in the way of recovery to be more balanced and/or helpful. This is an evidence based treatment used in my practice. I encourage folks to listen to this podcast episode when considering this treatment. Maybe not as well known as EMDR, but can be more effective.
- Prolonged Exposure Therapy (PE): Helps individuals gradually face trauma-related memories, emotions, and situations they have avoided since the trauma. These components are faced in safe environments. PE allows individuals to learn that trauma-related memories and cues are not dangerous and do not have to be avoided. This is the other evidence-based treatment for PTSD used in my practice.
- Eye Movement Desensitization and Reprocessing (EMDR): Involves guided eye movements to help process trauma.
- Medication: In some cases, medication may be used to manage symptoms like anxiety or depression associated with PTSD. NOTE: While medication can be part of the overall treatment for PTSD (usually medication and psychotherapy), medication is not a frontline treatment for PTSD. I cannot prescribe medication, but can refer to professionals who can, including psychiatrists, nurse practitioners, and primary care physicians.
Each approach addresses psychiatric treatment for post-traumatic stress in a unique way, providing options for people to find what works best for them. Here.is.Better. (need to include the link to their website) is a documentary showing the experiences of 4 veterans as they do CPT, PE, or EMDR through the VA. It gives a sense of what each treatment is like from the veterans’ perspectives.

Living with PTSD: What is PTSD Like?
Living with PTSD can feel overwhelming and unpredictable. For some, it may be marked by constant reminders of past events, while for others, it may manifest as chronic unease, vigilance, or even emotional numbness. Understanding what PTSD is like can foster empathy and encourage a more supportive environment for those who are impacted. Knowing that PTSD recovery is possible and that support exists is essential for anyone navigating this journey. The National Center for PTSD has a wealth of information for individuals with PTSD and their loved ones.
FAQs about PTSD
How does PTSD affect people?
PTSD can disrupt or worsen a person’s mental and physical health, strain relationships, and negatively affect them in their daily lives, leading to significant distress, impaired functioning, and lower quality of life. Those with PTSD have difficulty making sense of what happened. They may have negative thoughts about themselves, others, or the world, like “It’s my fault” or “I can’t trust anyone.” They may feel negative emotions, such as fear, anger, sadness, guilt, and/or shame. Or they may feel numb. They may avoid objectively safe/low risk situations/activities that they perceive as dangerous or threatening. They may avoid situations/activities/things that are objectively safe/low risk and remind them of the trauma. This can include avoiding sights as well as sounds, smells, andtouch/sensations. They may avoid social situations or doing things that they used to enjoy. They may have difficulties with trust and power/control. They may also experience depression, panic attacks, substance use, or other mental health issues.
How to tell if someone has PTSD?
Here are some potential signs to look for:
- Re-experiencing: May experience intense emotions and/or intense physiological reactions when they encounter trauma-related reminders, nightmares, intrusive memories
- Avoidance: Trying to avoid objectively safe/low-risk situations/activities that may remind them of the traumatic event, not engaging in activities they used to enjoy
- Negative changes in thoughts and mood: Withdrawing from/avoiding social situations, difficulty trusting self or others, negative self-views
- Hyperarousal: Constantly on guard, jumpy or easily startled, irritable
Please keep in mind that only a qualified mental health professional can provide an accurate diagnosis.
Can PTSD stay with you for life?
PTSD can be a long-term condition, but with proper assessment and treatment, symptoms can be managed effectively, allowing many to lead fulfilling lives. PTSD is not a life sentence. I cannot emphasize that enough.
How does PTSD make you act?
PTSD can cause people to act in various ways. They may be on guard and easily startled. They may be irritable and have trouble concentrating. They may have trouble falling asleep and/or staying asleep, separate from whether they are having nightmares. They may avoid thinking or talking about the trauma and avoid feeling emotions related to the trauma. They may avoid external reminders of the trauma, such as people, places, or things. Some may also experience a variety of emotions and struggle with trust.
Does PTSD qualify for disability?
PTSD can qualify for disability in some cases.
What happens if PTSD goes untreated?
Untreated PTSD can lead to chronic stress, depression, substance abuse, and worsening of mental health and physical health symptoms, impacting overall quality of life. It can strain relationships, negatively impact functioning in work/school, and lead to self-destructive behavior.
What usually triggers PTSD?
Triggers vary depending on the person, but often include reminders of the trauma, such as sights, sounds, smells, or bodily sensations; situations that invoke similar feelings of fear, anger, sadness, or helplessness; and negative thoughts of self, others, or the world.
What is the biggest symptom of PTSD?
Re-experiencing symptoms, like intrusive memories, nightmares, and flashbacks, as well as feelings of guilt and shame are some of the most commonly reported and impactful symptoms of PTSD.
Post-Traumatic Stress Disorder (PTSD) is a serious condition that affects millions worldwide, but awareness, understanding, and appropriate assessment and treatment can make a profound difference. It is not only limited to our soldiers or veterans. It affects civilians as well. That said, not all of the most effective treatment options are widely available for civilians, and I am here to change that (at least in NE Ohio). In Ohio, recent studies highlight the importance of addressing mental health trends to ensure everyone has access to the support they need. Whether you’re seeking help for yourself or a loved one, understanding ‘what is PTSD’ – is the first step in the journey to healing.
References
For more information on mental health trends in Ohio, explore the Ohio Health Policy Institute’s report and recent data snapshot to learn about the growing focus on mental wellness in the state.
American Psychiatric Association. (2013). Diagnostic and statistical manual of mental disorders (5th ed.). https://doi.org/10.1176/appi.books.9780890425596
Weathers, F.W., Blake, D.D., Schnurr, P.P., Kaloupek, D.G., Marx, B.P., & Keane, T.M.: (2013). The Clinician-Administered PTSD Scale for DSM-5 (CAPS-5) [Assessment]. Available from www.ptsd.va.gov
Weathers, F.W., Litz, B.T., Keane, T.M., Palmieri, P.A., Marx, B.P., & Schnurr, P.P. (2013). The PTSD Checklist for DSM-5 (PCL-5). Scale available from the National Center for PTSD at www.ptsd.va.gov.